
One of the common symptoms with which patients come to a medical facility is pain in the hip joint. The causes, treatment, and possible diseases that cause such a manifestation cannot be identified without qualified medical care. Discomfort in any part of the musculoskeletal system may indicate the development of serious pathologies, so dysfunction of the hip joint should not be ignored.
Anatomy of the hip joint area
The hip joint plays an important role in motor activity. This is one of the largest human joints, which can withstand heavy loads in a standing position, as well as during upright walking.
Bones that form a joint
The hip joint is formed by the head of the femur and the acetabulum of the innominate pelvic bone - the most powerful and largest parts of the human skeleton. The minimum number of anatomical elements of the joint ensures its strength and reliability, the ability to withstand body weight during movement. Most pathologies of the hip joint begin with damage to the acetabulum, the immobile part of the joint. It is shaped like a bowl, the center of which is directed upward at a slight angle, which ensures even distribution of the load between the pelvic bones.
The glenoid cavity is a strong and solid formation, which consists of 3 types of pelvic bones:
- ileal
- ischial
- pubic
The most vulnerable area of the articular cavity is in children whose bone tissue is not sufficiently strong. Due to the presence of a small bony ridge at the edge of the socket, the head of the femur is completely immersed in the "bowl", which provides strong support for the limb. The moving part of the joint is the femur (head, neck, greater and lesser trochanters). The shape of the head corresponds to the cavity of the articular cavity. It is covered with cartilage tissue, which ensures perfect alignment of the joint elements and their unhindered sliding. In the center of the head is a strong ligament that connects the bone to the acetabulum, providing additional grip and support.
The neck emerges from the head of the femur at an obtuse angle, which ensures mobility of the joint and uniform distribution of the load between the limbs. The trochanters are bony projections to which muscle tendons are attached.
Fabrics and structures
The normal functioning of the joint is ensured by a variety of structures, each of which performs corresponding functions.
Blood supply, performance and decreased sensitivity of the joint are provided by:
- Ligaments and tendons surround the joint on all sides, covering and protecting the femur and its neck, as well as the socket itself.
- Cartilage covers the head of the femur and part of the acetabulum.
- Subcartilaginous areas are bone tissue consisting of cells and connective extracellular substance.
- The joint membrane or capsule is the source of a special secretion - synovial fluid for lubricating the parts of the joint.
- The acetabular labrum connects the edge of the acetabulum and the transverse ligament.
The hip joint is supplied with nutrients through a fairly isolated network of vessels and arteries. The blood supply to the internal parts of the joint is provided by the acetabular branch of the obturator artery, and the capsules, ligaments and surrounding muscles are fed through the deep arteries of the thigh and buttocks.
Anatomical formations located next to the hip joint

Often the cause of pain in the hip joint is damage to the anatomical structures located next to it. These elements include:
- Skin and subcutaneous tissue - the outer covering of the body
- The muscles of the thigh, pelvis, lower back and buttocks provide joint mobility and additionally strengthen it from the outside
- Extra-articular ligaments - perform a strengthening function, located around the joint capsule
- Periarticular bursae are bundles of connective tissue that prevent friction between soft and hard tissues
Risk factors
Inflammatory processes in the pelvic area occur due to mechanical damage or damage to certain types of bacteria. In this case, both the elements of the joint and the anatomical formations surrounding them can be exposed to pathological effects.
As a rule, one or more structures become inflamed:
- leather
- muscles
- ligaments (extra-articular, femoral heads)
- periarticular bursae
- TBS capsule
- cartilage
- acetabular labrum
- subcartilaginous areas
Pain in the hip joint is often caused by harmful microorganisms that provoke the development of infectious arthritis. Other reasons are also common:
- immune system disorders
- joint injuries due to excessive physical activity
- old age
- metabolic disorders
- other diseases
Features of pain

When diagnosing hip pain, additional symptoms play an important role, which may indicate the root cause of the problem.
Pain in the hip joint and radiates to the leg
If pain from a sore joint radiates to the groin, knees or buttocks, then most likely the problem is caused by damage to the nerve innervating the leg area due to one of the following reasons:
- joint tumor
- infectious arthritis - occurs due to damage by a pathogen
- fracture of the femur (in the head or neck area)
- Legg-Calvé-Perthes pathology - necrosis of the cartilage tissue of the femoral head
- juvenile epiphysiolysis - disruption of the structure of the head of the joint and its inflammation
Pain in the hip joint, radiating to the leg, can signal pathologies of cartilage tissue and periarticular structures, lack of joint lubrication, and damage to the synovial membrane. Painful symptoms may occur suddenly or gradually increase.
Pain when walking
Pain in the hip joint can occur during walking if the acetabulum comes into contact with the cartilaginous tissue of the head of the femur, resulting in an inflammatory process. The cause of this phenomenon can be mechanical damage, inflammation of anatomical formations located next to the joint.
Based on the intensity of pain in the hip joint when walking, you can identify the root cause of the problem:
- discomfort that occurs at the beginning of walking, gradually subsiding - a sign of inflammation of the periarticular bursa
- discomfort that gradually increases from the moment you start walking - inflammation of the articular surfaces of the hip joint
- continuous pain of high intensity, accompanied by impaired functionality of the joint - occurs with dislocations and fractures
- pain occurs closer to night - a consequence of deformation of the cartilage of the femoral head and (or) acetabulum, which rub against each other and become inflamed
- pain of moderate intensity is a sign of minor injuries and bruises
Pain when abducting the leg
Pain when abducting the leg is caused by inflammation of the tissues and structures that provide movement: muscles, periarticular bursae, tendons. Similar symptoms often result from myositis (inflammation of muscle tissue), bursitis (inflammation of the periarticular bursa), and tendinitis (inflammation of the tendons).
Causes
In most cases, pain in the pelvic area is caused by the patient having one of the following problems:
- arthritis
- coxarthrosis
- bursitis of the trochanteric bursa
- tendinitis
- infectious pathologies
- inherited diseases
- tumor formation in the pelvic area
Without timely treatment, each of these causes can lead to severe complications, including loss of joint mobility.
Arthritis
Arthritis (coxitis) is a disease of joint tissue caused by disorders of the immune system or damage to pathogens: viruses and bacteria.
Arthritis symptoms:
- temperature increase
- pain and swelling in the joint area
- motor impairment
The disease occurs in acute, subacute and chronic forms.
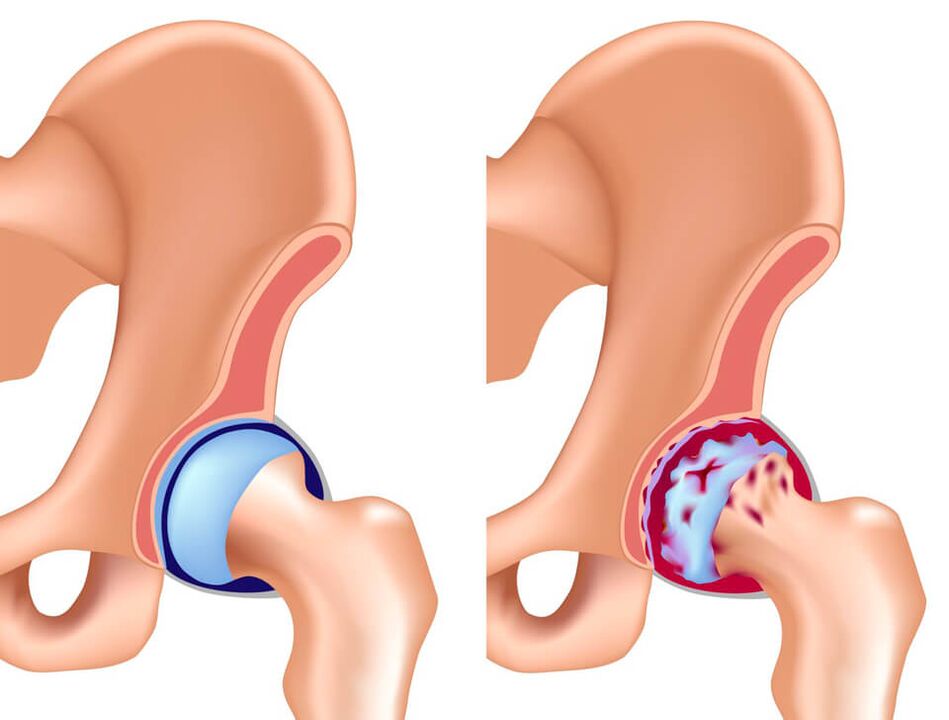
Coxarthrosis
Another name for coxarthrosis is osteoarthritis of the hip joint. This pathology is caused by metabolic disorders in cartilaginous tissues, resulting in their death. The cause of this phenomenon may be injury, impaired blood supply, excessive physical activity, age over 45 years, and heredity. The main symptom of coxarthrosis is pain in the lower back, groin, and buttocks, which gradually increases during physical activity and leads to lameness. Discomfort decreases during periods of inactivity.
Bursitis of the trochanteric bursa

The presence of an inflammatory process in the bursa (trochanteric bursa) is characterized by the occurrence of intense pain in the joint area. Athletes and elderly people are susceptible to the disease. The main symptom of bursitis of the trochanteric bursa is pain in the area of the greater trochanter, which increases when trying to lean on the affected leg.
Tendinitis
Inflammation of the tendons is called tendinitis. This is a disease that occurs in acute or chronic forms and leads to degenerative changes in tissue. Often the pathology occurs in athletes who do not follow their running technique, as well as after heavy load on the hip muscles.
Typically, tendinitis is a complication of another disease:
- thyroid pathology
- metabolic disorders
- arthritis
- arthrosis
- inflammatory process of systemic or infectious origin
- hip dysplasia
Tendonitis causes the patient discomfort during movement, pain, changes in gait, and clicking when walking in the joint area.
Infections
Some infectious diseases cause inflammation of the joint tissues, as well as nearby anatomical structures, resulting in intense pain in the hip joint. Most often, the following pathologies have similar symptoms:
- Aseptic necrosis of the femoral head is a disruption of the blood supply to the groin area, resulting in tissue death. The pain associated with this disease is acute and intense. The problem is more common in males.
- Purulent arthritis is a serious disease that requires immediate treatment. If you do not seek medical help promptly, sepsis may occur. Associated symptoms are general intoxication, pain and swelling in the area of the affected joint, difficulty in motor activity.
- Tuberculous arthritis is common in children and is characterized by a slow progression. Associated symptoms are increased fatigue, decreased motor activity, and muscle atrophy. Pain of varying intensity increases when a purulent abscess occurs.
Infectious pathologies of the hip joint lead to severe complications and therefore require immediate treatment.
Hereditary diseases

Hereditary pathologies of the hip joint usually appear between the ages of 1 and 10 years, and are characterized by pathological changes in the tissue of the glenoid cavity and/or head of the femur. The most common hereditary disease affecting the hip joint is Legg-Calvé-Perthes syndrome, which is characterized by pain and gait disturbance due to the death of the cartilage tissue of the joint.
Tumors of bones and soft tissues
Benign or malignant growths of bone and soft tissue in the hip joint can cause pain when walking or at rest. The tumor can occur in bone tissues (osteomyelitis), cartilaginous tissues (chondroblastoma, chondroma), osteochondral tissues (osteochondroma). As a rule, neoplasms cause discomfort and are felt upon palpation. Benign tumors are treated surgically; some of them can transform into cancerous tumors.
Soft tissue tumors of the thigh:
- lipoma
- rhabdomyoma
- fibroma
- hemangioma
- neuroma
An oncologist is involved in the diagnosis and treatment of tumors in the hips and pelvis.
What to do
With severe pathologies of the hip joint, a person feels severe pain. Discomfort in the pelvic area is a reason to visit a medical facility for examination and treatment.
Particular attention should be paid to the intensity of pain:
- Lungs- occur with bruises after an injury. Cold should be applied to the sore area to reduce swelling. To reduce pain, it is recommended to take a non-steroidal anti-inflammatory drug. It is advisable to consult a doctor.
- Moderate- usually occur in diseases of the hip joint, accompanied by difficulty in motor activity and increased body temperature. Discomfort increases during physical activity. It is necessary to consult a rheumatologist.
- Strong- arise due to dislocations and fractures. Accompanied by limitation or impossibility of physical activity. In cases of severe pain in the hip joint caused by injury, you should contact an ambulance.
There are many folk recipes that are used for pain in the hip joint. It is important to remember that all of them are suitable for symptomatic treatment and pain reduction, but will not help eliminate the cause of the problem. Effective treatment is carried out exclusively under the supervision of a qualified physician.
Which doctor should I contact?

If you have pain in the hip joint, you should contact your family doctor or general practitioner, who will refer you to a specialist. Diseases of the musculoskeletal system are dealt with:
- traumatologist— pain in the hip joint due to physical activity, sprains, falls and other injuries
- rheumatologist- sudden onset of joint pain for no apparent reason
You may also need to consult other doctors: a surgeon, oncologist, infectious disease specialist, etc.
Diagnostics
The first important stage in diagnosing pain in the hip joint is an external examination, which necessarily includes taking an anamnesis and palpation. Depending on the severity of the disease and the patient’s complaints, laboratory tests and instrumental diagnostic methods are prescribed:
- radiography- the use of x-rays to examine a specific area of the body
- CT and MRI- modern accurate diagnostic methods that allow you to obtain highly informative images of the joint and the area around it
- microbiological examination of a sample of biological materialallow to detect the presence of pathogenic microorganisms: viruses and bacteria
- immunological blood test- allows you to identify immune disorders, determine the presence of certain autoantibodies
- arthroscopy (endoscopic examination)— examination using a probe, the possibility of taking a sample of joint tissue for further research
- laboratory examination of effusion- taking a sample of intra-articular fluid during puncture and identifying the causative agent of an infectious disease in it, checking for sterility
The use of several diagnostic methods in combination allows us to identify the cause of pain in the hip joint with high accuracy.
Treatment

Treatment of pain in the hip joint should be prescribed by a doctor based on the examination and diagnosis. As a rule, drug therapy or surgery is prescribed.
Medication
Treatment of pain in the hip joint should be comprehensive, aimed at eliminating symptoms, and most importantly, eliminating the cause of the problem. For this purpose, drug therapy is used, which includes the use of:
- non-steroidal anti-inflammatory drugs- help reduce pain, relieve swelling
- means to improve microcirculation- help restore blood circulation and nutrition of joint tissues
- chondroprotectors- promotes the restoration of cartilage tissue
- muscle relaxants- reduce pain, improve blood flow in the damaged area
- hormonal drugs- to relieve pain and suppress inflammation
In the treatment of pain in the hip joint, physiological procedures are highly effective: massage, acupuncture, cryo- and laser therapy. Special therapeutic exercises and manual therapy are also used.
Surgical
Surgical intervention is indicated in advanced cases when conservative treatment does not help the patient. This involves partial or complete replacement of the diseased joint with a prosthesis.
Prevention
Reducing the load on the legs will slow down the pathological processes inside the joint, so people who are obese are recommended to start losing weight.
Preventive measures will help reduce pain in the hip joint:
- regular walking
- physiotherapy
- a balanced diet rich in vitamins A, C, E
Timely consultation with a doctor in the first stages of the disease increases the effectiveness of treatment and also reduces the risk of complications and serious consequences for the body.

















































